Prediabetes
Everything you need to know
Prediabetes and type 2 diabetes are metabolic diseases that are becoming increasingly prevalent.
Globally, there are more than 422 million people with diabetes compared to around 108 million in 1980. In the UK, almost 3.7 million people have been diagnosed with diabetes but it is estimated that the total number of people with diabetes is closer to 4.6 million.
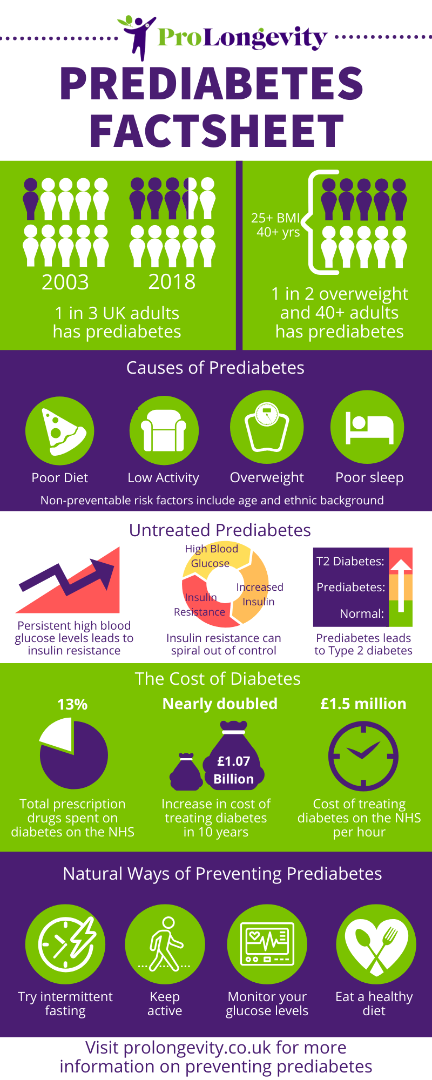
In England, 1 in 3 adults has prediabetes. However, this number was closer to only 1 in 10 adults in 2003. Estimates suggest that 50% of all people who are overweight and over 40 years of age have prediabetes.

Prediabetes is a condition where blood glucose levels are higher than normal. Left untreated, the glucose levels may increase further. This is when prediabetes develops into type 2 diabetes.
However, treating prediabetes is possible. Taking action and having prediabetes treatment can reverse the condition and help prevent the onset of type 2 diabetes.
Other names for prediabetes include early-stage diabetes, borderline diabetes, insulin resistance, impaired fasting glucose (IFT) or impaired glucose tolerance (IGT).
Many factors contribute to the risk of developing prediabetes. However, an unhealthy lifestyle is the biggest cause.
An unhealthy lifestyle can be described as having:
- A poor diet
- Low activity levels
- Excess weight
- Poor quality of sleep
However, there are other risk factors you cannot control:
- If you have a family history of diabetes
- Having Hispanic, African or a Pacific Islander racial heritage
- Being older than 45
- Having had gestational diabetes or a baby who weighed over 9 pounds (4.1 kg)
- Having polycystic ovary syndrome or obstructive sleep apnea
You cannot control these risk factors so it’s important to make healthy lifestyle choices to reduce your risk of developing prediabetes.
Most people with prediabetes don’t know they have it. This is because many people will not experience any symptoms. Those that do may find themselves:
- Being thirstier than normal
- Needing to go to the toilet more frequently
- Feeling tired
- Blurry vision
- Having skin tags or Acanthosis Nigracans
There are often no signs to warn that you have prediabetes. It’s only when the condition develops into type 2 diabetes that symptoms begin. By which time it may be too late to prevent the onset of full diabetes.
If you or your doctor suspects you have prediabetes, you will most likely be given a blood test. There are two types of blood tests you can have to diagnose prediabetes:
- The fasting plasma glucose test measures how much glucose is in your blood after a period of fasting (not eating).
- The HbA1c test measures the numbers of glycated red blood cells a.k.a. red blood cells that have bonded to glucose.
Another way to diagnose prediabetes is the oral glucose tolerance test (OGTT). You are given a sugary drink and your blood glucose levels are monitored over the next few hours to see how you respond.
You will have prediabetes if:
- Your fasting plasma glucose is between 5.5 and 6.9
- Your HbA1c count is between 42 and 47 (can also be expressed as between 6.0% and 6.5% )
Any results above these levels and you will either be diagnosed with type 2 diabetes or be given a different test to confirm diabetes.
You may hear your doctor talk about impaired fasting glucose (IFT). This means after some time without eating, your blood sugar levels are abnormally high.
Impaired glucose tolerance (IGT) means soon after eating, the spike in blood sugar is abnormally high.
Yes, once diagnosed prediabetes is reversible with the correct changes to your diet and lifestyle.
These changes may include:
- Avoiding sugar in the diet
- Reducing the amount of carbs you eat
- Taking daily or regular exercise
- Eating a diet low in processed foods
- Reducing your alcohol intake
- Losing weight
- Avoiding sedentary behaviour
Your doctor will also recommend you stop smoking if you haven’t already done so.
Left untreated, prediabetes can develop into type 2 diabetes. Each year, around 5 to 10% of people with prediabetes will develop type 2 diabetes.
Type 2 diabetes cannot be cured but it can be managed and possibly reversed. However, it can be a life-long, chronic condition that will have profound consequences to your health.
Type 2 diabetes is linked to many serious health conditions:
- Heart disease, stroke and hypertension
- Nerve damage to fingers and toes that may eventually affect the whole limb
- Erectile dysfunction in men
- Kidney damage leading to kidney failure
- Eye disease including blindness
- Hearing impairment and deafness
- Alzheimer’s disease
- Some cancers
- Reduced life expectancy
Preventing type 2 diabetes is significantly better than living with type 2 diabetes. Even if the condition is properly managed, anyone with type 2 diabetes can expect some kind of significant impact on their health including dying up to 10 years earlier.
The cost of treating diabetes
According to NHS Digital, the cost of treating diabetes has almost doubled in the last ten years from £650 million to a staggering £1.07 billion in 2018/19. Diabetes medicines account for nearly 13% of the total cost of prescribing for England – more than any other condition.
Catching prediabetes early, before it turns in type 2 diabetes is therefore paramount for the individual and the NHS.
Your body constantly works at maintaining balance.
The process is called homeostasis and includes regulating your body temperature, water content and carbon dioxide levels. Most processes use negative feedback mechanisms to achieve this stability.
Your blood sugar levels are maintained in this way by two chemicals, called insulin and glucagon, that can lower or raise your blood glucose amounts as needed.
Glucose is a sugar that is your primary energy source. Glucose comes from the sugar and carbohydrates in the food you eat.
During digestion, your small intestine absorbs glucose and passes it into your bloodstream. From here, it can be used immediately as fuel for the body. Any excess, ie beyond what the body needs to burn straight away as fuel, can be stored in two ways: As glycogen (in the liver and the muscles) or as fat in the body’s fat stores (or adipose tissue) stores. Both stored glycogen and stored fat can be used when the body needs more fuel.
The most glucose-hungry organ is your brain. If you’re hungry or haven’t eaten for a while you may get grumpy or find it hard to concentrate. This is what happens when your brain wants more glucose.
However, people who experience long-term inconsistent glucose levels, such as diabetics, are at risk of developing cognitive conditions such as dementia.
So, maintaining the right amount of glucose in your blood is important for brain health and many other aspects of your wellbeing. Controlling this healthy amount of glucose in your bloodstream is managed by insulin and glucagon.
Insulin is a hormone that your pancreas produces. Insulin is released in response to increases in blood glucose levels, such as after eating. The role of insulin is to remove excess glucose from your blood by allowing it to cross into your body’s cells.
When sufficient glucose has been removed from your bloodstream, the pancreas will stop producing insulin. Therefore, insulin helps prevent blood glucose levels from getting too high.
Conversely, if your blood sugar levels drop too low, another hormone called glucagon comes into play. Glucagon is also produced by the pancreas and tells your liver to release glucose, stored as the fatty glycogen, into your bloodstream. Therefore, glucagon helps prevent your blood glucose from getting too low.
Insulin is released more frequently and in greater amounts to combat long-term high blood sugar levels. The cells become over-exposed to insulin and eventually less receptive to it. The cells have become accustomed to the constant presence of insulin and therefore resistant to insulin’s signal. This is insulin resistance.
Insulin resistance is a feedback loop that can spiral out of control if left untreated.
Because insulin-resistant cells aren’t absorbing as much glucose for fuel, the body experiences fatigue. If you’re low on energy you may eat more carb-rich foods that increase your blood glucose. This triggers the release of more insulin and the already apathetic cells become even more resistant to insulin. Your cells absorb less glucose and the cycle continues.
Insulin resistance is another term for prediabetes.
The balance of other hormones are also disrupted:
- Ghrelin is the hunger hormone that reminds you to eat. High-carb foods only switch ghrelin off for short periods of time and so you will feel hungrier more often.
- Fat cells secrete a hormone called leptin that tells you when you’re full. However, escalating amounts of insulin overwhelm the cells making them ignore the leptin signal. You may become leptin-resistant which often leads to weight gain.
The result is insulin, ghrelin and leptin working against each other rather than in harmony. Your body’s balancing act becomes unstable. You’re permanently hungry, tired and overweight.
Normally, excess glucose is stored as glycogen, thus removing it from your bloodstream. However, if your insulin levels are insufficient or your body is insulin resistant, too much glucose remains in your blood.
If blood glucose levels remain high for extended periods of time, they can affect the proper functioning of your body.
- Your body will try to flush the excess glucose out through your urine – making you pee more often.
- The glycogen fuel reserves become over-full resulting in fatty liver disease.
- The liver becomes inflamed and presses on the pancreas, limiting the amount of insulin the pancreas can produce.
- Insulin resistance increases.
- Your body cannot regulate its blood sugar levels and develops type 2 diabetes.
Type 1 diabetes is an auto-immune condition where someone cannot produce enough effective insulin. Sometimes this is from childhood but it can develop during adulthood. People with type 1 diabetes need to inject themselves with insulin to help maintain their blood glucose levels.
Type 2 diabetes is a condition that has traditionally developed as you get older but we is becoming increasingly common in younger people and even teenagers. Type 2 diabetes is both preventable and reversible. It is when your body becomes less reactive to insulin and is treated with a restrictive diet and medications, such as metformin, to reduce your blood glucose amounts.
However, Type 1 diabetes is much rarer than type 2 diabetes: only around 8% of the diabetic population has type 1 diabetes.
The reasons for the increase in prediabetes and diabetes are more complicated than just poor lifestyle although these are an important concern:
- Easy access to processed foods
- Increasing obesity
- Consumption of fruit and vegetables is decreasing
- Ageing population
- Poor sleeping habits
This ageing population means two things:
- The risk of developing prediabetes or type 2 diabetes increases as we age so a bigger proportion of adults are likely to have diabetes.
- Our ability to treat and manage type 2 diabetes is improving and so diabetics are living longer.
It’s important to note that living longer does not always mean living with a good quality of health. Despite being able to manage type 2 diabetes, it is still a chronic condition that, left to its own devices, can blight your senior years.
Environmental factors, such as increasing air pollution from car fumes and pesticides, may also contribute to the rise in diabetes.
If you are overweight and over 40 years of age, you’re very likely to already have prediabetes. The only way to be sure is to have a blood test.
As well as regular exercise and healthy eating, here are some other simple ways to help naturally prevent or treat prediabetes:
- Eating a low-carb or low GI diet
- Avoid processed foods
- Try intermittent fasting or giving yourself a 12-hour eating break between dinner and breakfast
- Having a regular blood test or monitor your blood glucose levels
- Drinking plenty of water
- Aim for at least 8 hours of sleep each night





